Understanding RateFast from a high level will help users communicate their impairment reports to other stakeholders. Dr. John Alchemy, creator and CEO of RateFast, explains how this knowledge can lead to closing work comp claims quicker than ever before.
Data Integrity: Understanding Foundational Clinic Data
Good data integrity means a report that is more likely to stand on its own when scrutinized. What does it mean for your impairment report data to have integrity? Data integrity is a concept we’ve developed at RateFast which represents the quality of the data that was put into the creation of the report, since the outcome of a report is only as good as the data that was provided.
Data integrity is provided with each RateFast report as a means to keep the claim as transparent as possible for stakeholders.
Continue reading Data Integrity: Understanding Foundational Clinic Data
Apportionment: Understanding the Drivers of Pre-Existing Conditions
Dr. John Alchemy discusses one of the most difficult parts of workers’ compensation impairment ratings: Apportionment. When a workers’ compensation injury involves a pre-existing condition on the injured body system, the physician must calculate apportionment to determine how much functional loss was due to the workplace injury, and how much of it is owed to the pre-existing condition. Dr. Alchemy will outline how to navigate through this particularly tough topic for the best outcome for impairment rating.
If you’re a workers’ compensation provider, adjuster, or case manager check out RateFast Express: the service that writes your impairment reports with you!
Questions? Comments? Suggestions for podcast episodes? Reach out to us anytime at caworkcompreport@rate-fast.com!
Connect with RateFast CEO Dr. John Alchemy on LinkedIn!
RateFast Podcast: A Nurse Case Manager’s Guide to RateFast Express
This week we give a rundown of the ways that RateFast Express can be helpful to the workload of workers’ comp Nurse Case Managers. We discuss things such as the ways that RateFast Express speeds up claims, as well as how to sign up for and start using RateFast Express today!
If you’re a workers’ compensation provider, adjuster, or case manager check out RateFast Express: the service that writes your impairment reports with you!
Questions? Comments? Suggestions for podcast episodes? Reach out to us anytime at caworkcompreport@rate-fast.com!
We Asked the AI “What is RateFast”
Recently, we asked the now ubiquitous ChatGPT AI language model a question that many now-devout work comp professionals asked once upon a time: “What is RateFast?”
Here was its response:
Continue reading We Asked the AI “What is RateFast”
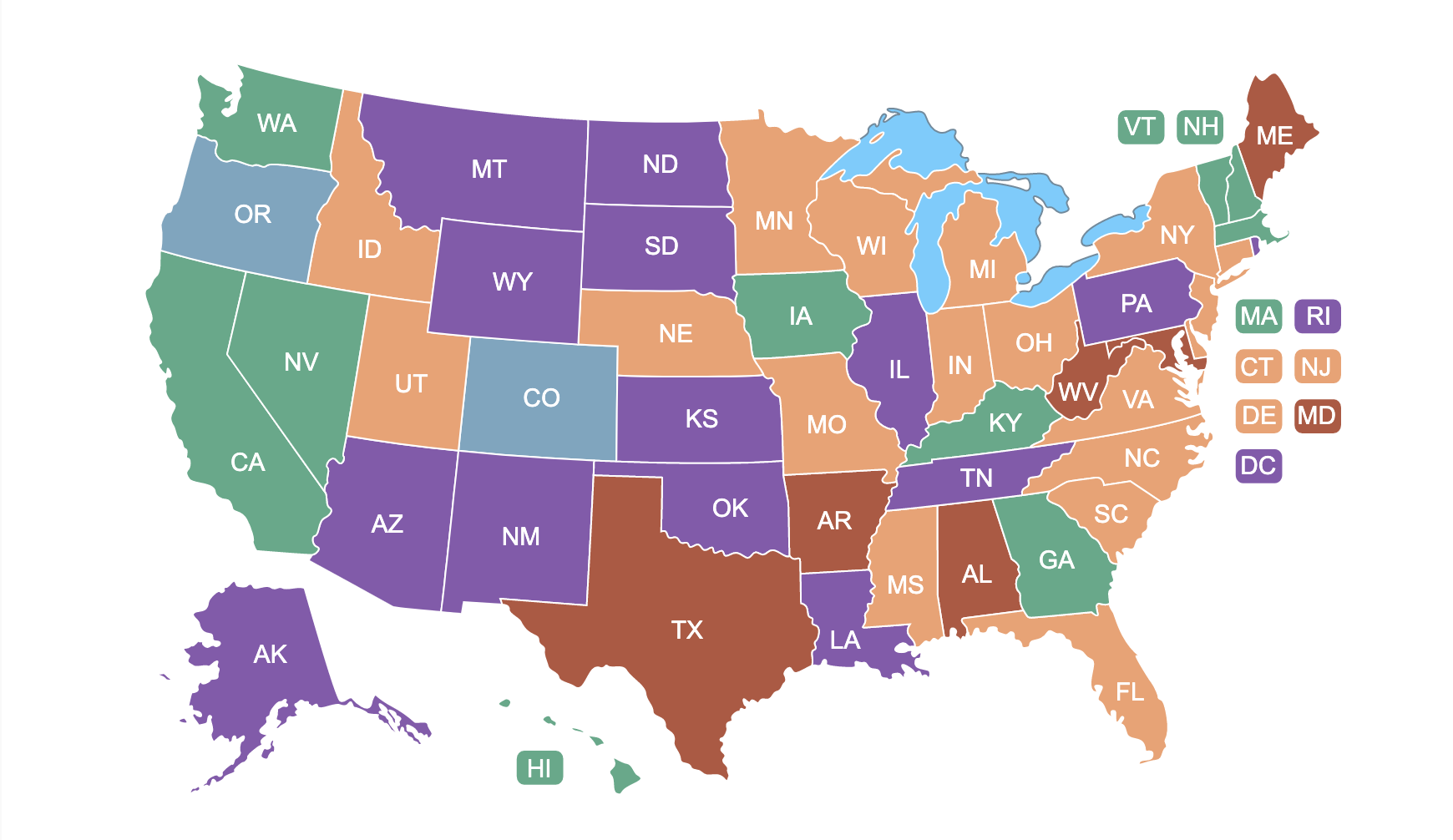
Reminder: We Have an Interactive Map of the Work Comp Rules in the United States!
Click here to go to our US Map of Workers’ Compensation!
Have you ever wondered what version of the AMA guides are used in South Dakota? How many states use a state specific ruleset for determining impairment? What is the oldest version of the AMA Guides in use?
Whether you need a question answered for your workers’ comp practice, or you’re just plain curious, we have a map for you!
The RateFast US Map of Impairment Rules
back in 2018 we put this map together to give any party in a work comp claim access to their state’s rule set, as well as some resources that will help them smooth the work comp process.
5 years later, we are still maintaining that US map, and want to make sure that you know that it’s there!
Updates
We have recently updated the map with a helpful key, in order to more clearly read the map and find your state’s ruleset.
It is also important that we make sure that the map is always up to date, so we make an effort to regularly maintain our map page.
Conclusion
Sometimes work comp providers operate in a different state than their patient’s injury. Adjusters and other parties often work across state lines. There are many situations where one might need a US map of workers’ comp state rules, and we’re happy to provide it!
RateFast Podcast: Interview with Dan Anders of Tower MSA Pt. II
In this final episode in our series with Dan Anders, Chief Compliance Officer of Tower MSA, we talk about what MSAs (Medicare Set Asides) are in general, and how they are applied in workers’ compensation. Mr. Anders also has his own podcast called Set Aside Some Time where he delves even further into the world of MSAs.
If you’re a workers’ compensation provider, adjuster, or case manager check out RateFast Express: the service that writes your impairment reports with you!
Work Comp Win: RateFast Receives a Patent!
Every day, people come up with quite useful ideas. Some of the ideas are genius. The problem is that nobody will ever know that the idea is genius if they never see it!
And simply because one has a great idea, it doesn’t necessarily mean that the idea is eligible for a patent.
To go along with the benefits of having the government recognize the fruits of your labor, there’s a certain… je ne sais quoi about having an official patent for a product that you’ve made. Suffice to say, RateFast is quite pleased that we have patented our product!
Continue reading Work Comp Win: RateFast Receives a Patent!
Workers’ Compensation Hell: Getting Through to the Other Side
This post is based on a five-part podcast series that we did with art historian Paul Costa covering the topic Dante Alighieri, his seminal work Inferno, 1800s French sculptor Auguste Rodin, and his famous piece The Gates of Hell. We encourage you to check it out!
Injured workers who have spent enough time stuck in the workers’ compensation system very well may refer to their experience with the process as hell.
We’re referring to claims that have dragged on for 6 – 10 months and beyond. The harrowing experience of being stuck in the claim can be equal to, and sometimes worse, than the workplace injury itself.
Here we examine just how these work comp claims can be like hell, specifically from the perspective of Dante’s work, Inferno.
Continue reading Workers’ Compensation Hell: Getting Through to the Other Side
RateFast Podcast: Radiculopathy Revisited
Is it radical? Is it ridiculous? It’s radiculopathy! One of our favorite words here in workers’ compensation, if nothing else, because it’s just fun to say. Dr. John Alchemy and Cory Oleson are discussing the ‘root’ of radiculopathy pain and some of the truths and not-so-truths about radiculopathy!
If you’re a workers’ compensation provider, adjuster, or case manager check out RateFast Express: the service that writes your impairment reports for you!