This article is for medical providers, insurance adjusters, and attorneys who want to better understand the process of a Sub Rosa within the context of a workers’ compensation case.

What is a Sub Rosa?
Sub Rosa is a fancy latin term that literally means “Under the Rose.” In workers’ compensation, however, it means secret investigation—surveillance. During a Sub Rosa investigation, usually an investigator is sent out to survey the injured worker. The investigator attempts to observe what level of physical activity the injured worker can or cannot perform. The second, and less common use of Sub Rosa in work comp is to investigate a doctor, an employer, work sites, and/or working conditions.
What are the stakeholders looking for in a Sub Rosa?
When insurance adjusters, employers, or medical providers require a Sub Rosa investigation, they are normally looking evidence that an employee can perform observable physical activities that are in excess of what they claim they can do.
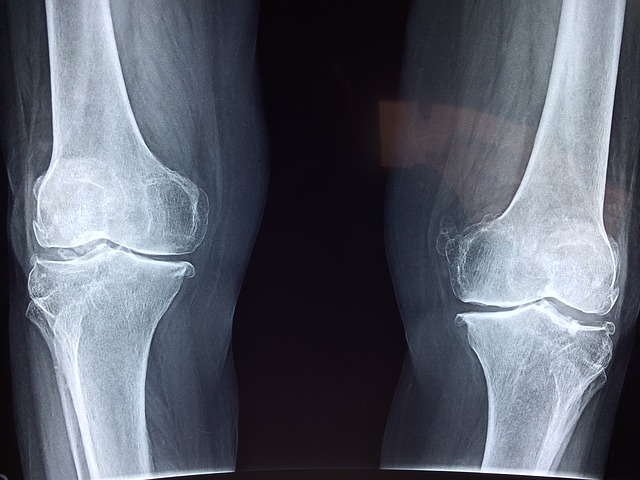
For instance, an injured worker may report that they can’t lift anything, or can’t bend over, or can’t walk without a cane. The fundamental purpose of this surveillance is to verify or disprove the validity of what the person is claiming in regards to their physical or psychological conditions.
Sometimes a patient may claim that they have good days and bad days. In these cases, their limitations ambiguous. It’s very important, therefore, that Sub Rosas span several, separate days, to provide an accurate view of the patient’s conditions.
What should the doctor do while viewing surveillance footage of a patient?
Most surveillance tapes are dead-boring. It is advisable for the doctor to dictate what she observes the patient doing while she watches the tape. It’s also important for the doctor to state whether she can clearly identify that the person being filmed is the patient in question, or whether she knows it is certainly not the patient, or whether she can’t tell.
When should an attorney consider requesting a Sub Rosa?
An attorney may consider a Sub Rosa to be useful if one or more of the following are present:
- Is the patient off from work for a much longer time than is typical for their condition?
- Does the patient have a history of workers’ comp cases where this has been a trend?
- Do physical findings corroborate with the patient’s description of their symptoms?
Should a doctor confront the patient with apparent discrepancies before recommending a Sub Rosa?
Yes. There is a lot that can be gained from a frank discussion with the patient about their symptoms and physical findings. Here at RateFast, we are committed to remaining non-partisan—we believe the ultimate goal of a workers’ compensation claim should be to get patients safely back to work. Therefore, we recommend an open and honest discussion with the injured worker before considering surveillance.
Try RateFast Express today!